The Impact of Food Insecurity on Health
June 27, 2016
Food insecurity – the inadequate or insecure access to food due to financial constraints – is a serious public health problem in Canada. It negatively impacts physical, mental, and social health, and costs our healthcare system considerably.
Statistics Canada began monitoring food insecurity in 2005 through the Canadian Community Health Survey (CCHS). Since then, food insecurity has persisted across Canada, with over 4 million Canadians living in food insecure households.
Food-insecure individuals, both adults and children, are likely to have poorer health.
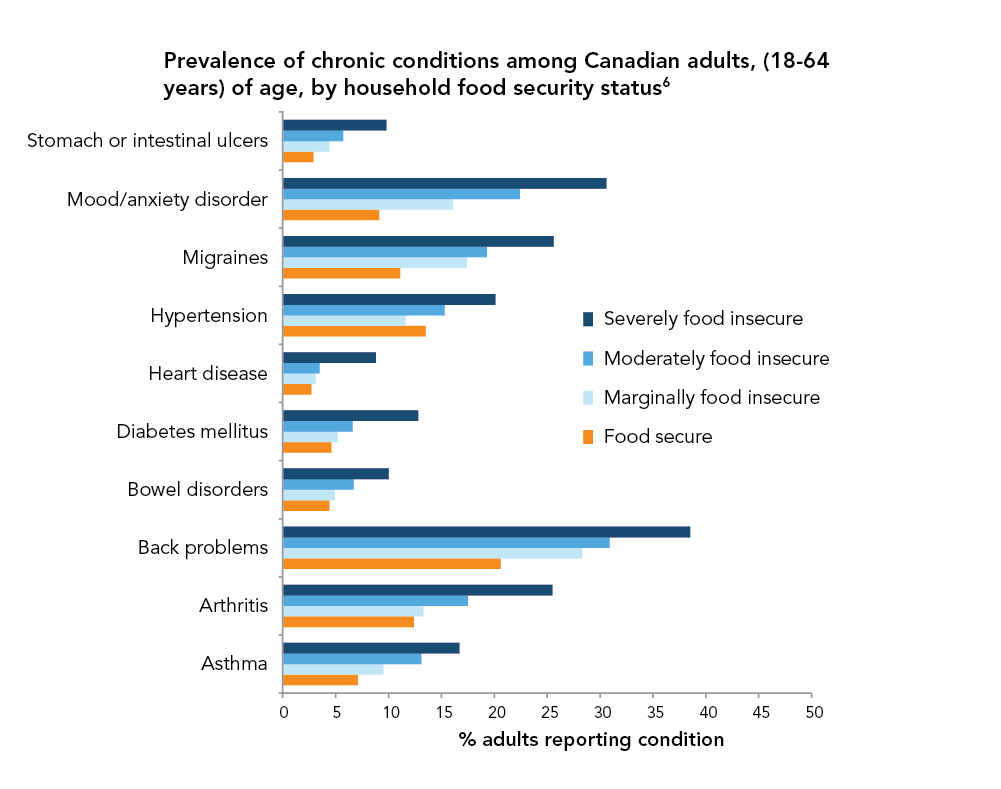
Food-insecure adults are more vulnerable to chronic conditions, with the risk increasing with the severity of food insecurity.1
Exposure to severe food insecurity leaves an indelible mark on children’s wellbeing, manifesting in greater risks for conditions like asthma, depression, and suicidal ideation in adolescence and early adulthood.2, 3
Food insecurity also makes it difficult for individuals to manage existing chronic health problems, such as diabetes and HIV.4, 5
Due to scarce resources, food insecure individuals may forego critical expenses like medication.
Health care costs
Household food insecurity takes a tremendous toll on the health care system.7
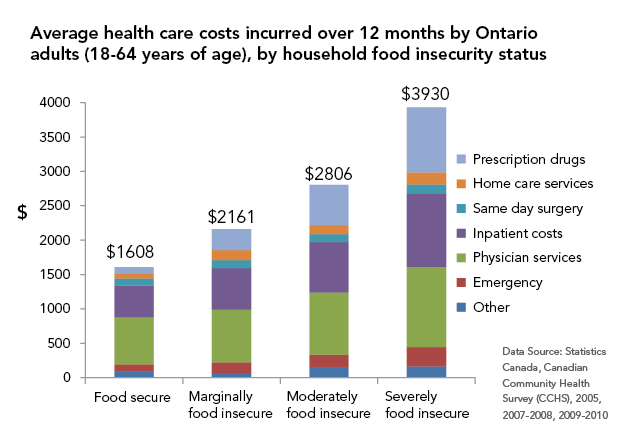
After adjusting for other well-established social determinants of health, such as education and income levels, total annual health care costs in Ontario were:
- 23% higher for adults living in marginally food insecure households than in food secure households
- 49% higher for adults living in moderately food insecure households than in food secure households
- 121% higher for adults living in severely food insecure households than in food secure households
These findings imply that addressing food insecurity through targeted policy interventions would reduce the associated health care costs and improve overall health.
References
- Vozoris, N. T., & Tarasuk, V. S. (2003). Household food insufficiency is associated with poorer health. J Nutr, 133(1), 120-126. http://jn.nutrition.org/content/133/1/120
- Kirkpatrick, S. I., McIntyre, L., & Potestio, M. L. (2010). Child hunger and long-term adverse consequences for health. Arch Pediat Adol Med. 164(8), 754-762. http://archpedi.jamanetwork.com/article.aspx?articleid=383613&
- McIntyre, L., Williams, J. V., Lavorato, D. H., & Patten, S. (2013). Depression and suicide ideation in late adolescence and early adulthood are an outcome of child hunger. J Affect Disorders. 150(1), 123-129. http://www.sciencedirect.com/science/article/pii/S0165032712007823
- Chan J, DeMelo M, Gingras J, Gucciardi E. Challenges of Diabetes Self-Management in Adults Affected by Food Insecurity in a Large Urban Centre of Ontario, Canada. Int J Endocrinol. 2009; 32(12), 2218-2224. http://www.hindawi.com/journals/ije/2015/903468/abs/
- Anema, A., Vogenthaler, N., Frongillo, E. A., Kadiyala, S., & Weiser, S. D. (2009). Food insecurity and HIV/AIDS: current knowledge, gaps, and research priorities. Current HIV/AIDS Reports, 6(4), 224-231. http://link.springer.com/article/10.1007/s11904-009-0030-z
- Tarasuk V, Mitchell A, McLaren L & McIntyre L. (2013) Chronic physical and mental health conditions among adults may increase vulnerability to household food insecurity. J Nutr. 143(11), 1785-93. http://jn.nutrition.org/content/early/2013/08/26/jn.113.178483
- Tarasuk, V., Cheng, J., de Oliveira, C., Dachner, N., Gundersen, C., & Kurdyak, P. (2015). Association between household food insecurity and annual health care costs. Can Med Assoc J. 187(14), E429-E436. http://www.cmaj.ca/content/early/2015/08/10/cmaj.150234