Food Insecurity and Mental Health
February 22, 2018
Household food insecurity – the inadequate or insecure access to food due to financial constraints – is a serious public health problem in Canada. It negatively impacts physical, mental, and social health, and costs our health care system considerably.
Statistics Canada began monitoring household food insecurity in 2005 through the Canadian Community Health Survey (CCHS). Since then, it has persisted across Canada. From the most recent national estimate, 1 in 8 households in Canada is food insecure, amounting to over 4 million Canadians, including 1.15 million children, living in homes that struggle to put food on the table.
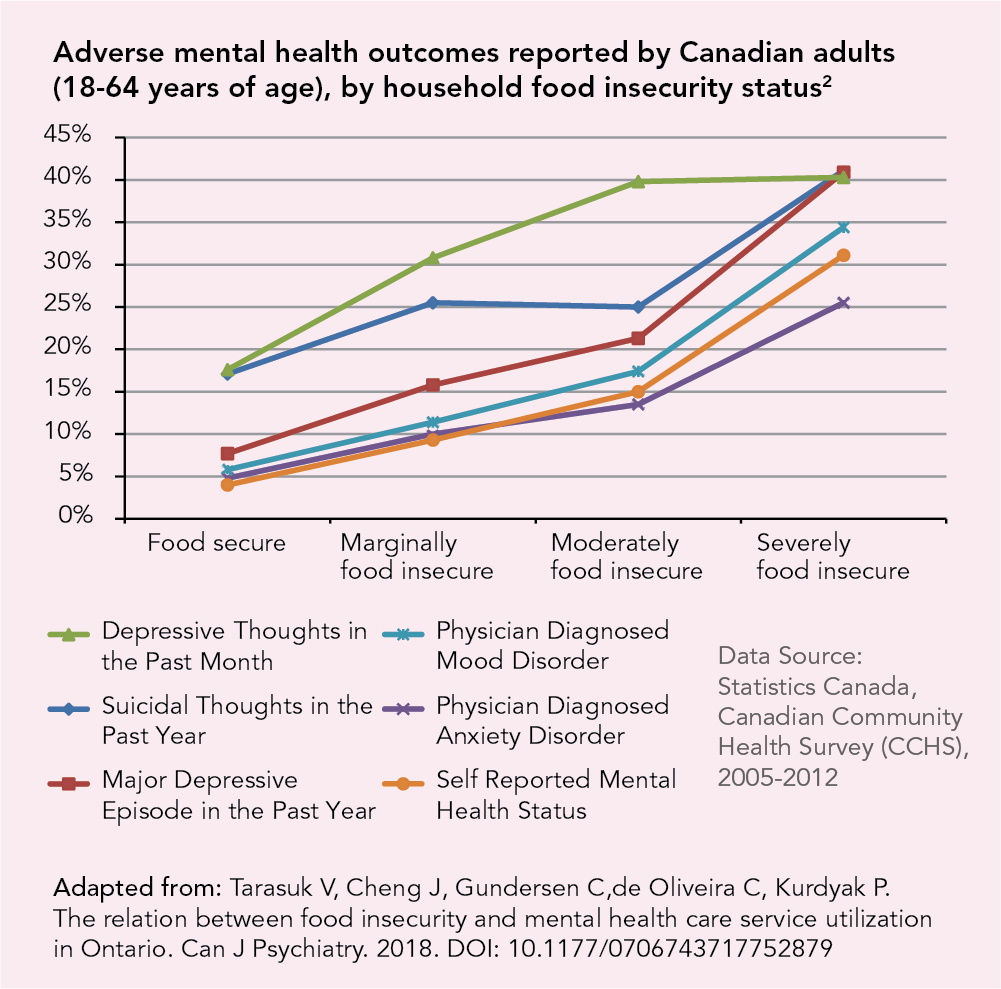
Household food insecurity is strongly related to mental health. Canadians living in food insecure households are at greater risk of poor mental health than those living in food secure households and this risk increases with the severity of food insecurity.1, 2 The health consequences of food insecurity take a large toll on our health care system.3, 4
Adults living in food insecure households are more likely to experience a wide range of adverse mental health outcomes, compared to those living in food secure households.2
For children, living in a food insecure household is associated with childhood mental health problems like hyperactivity and inattention.5
Experiences of hunger during childhood have a serious and lasting impact on mental health, manifesting in greater risks of depression and suicidal ideation in adolescence and early adulthood.6, 7
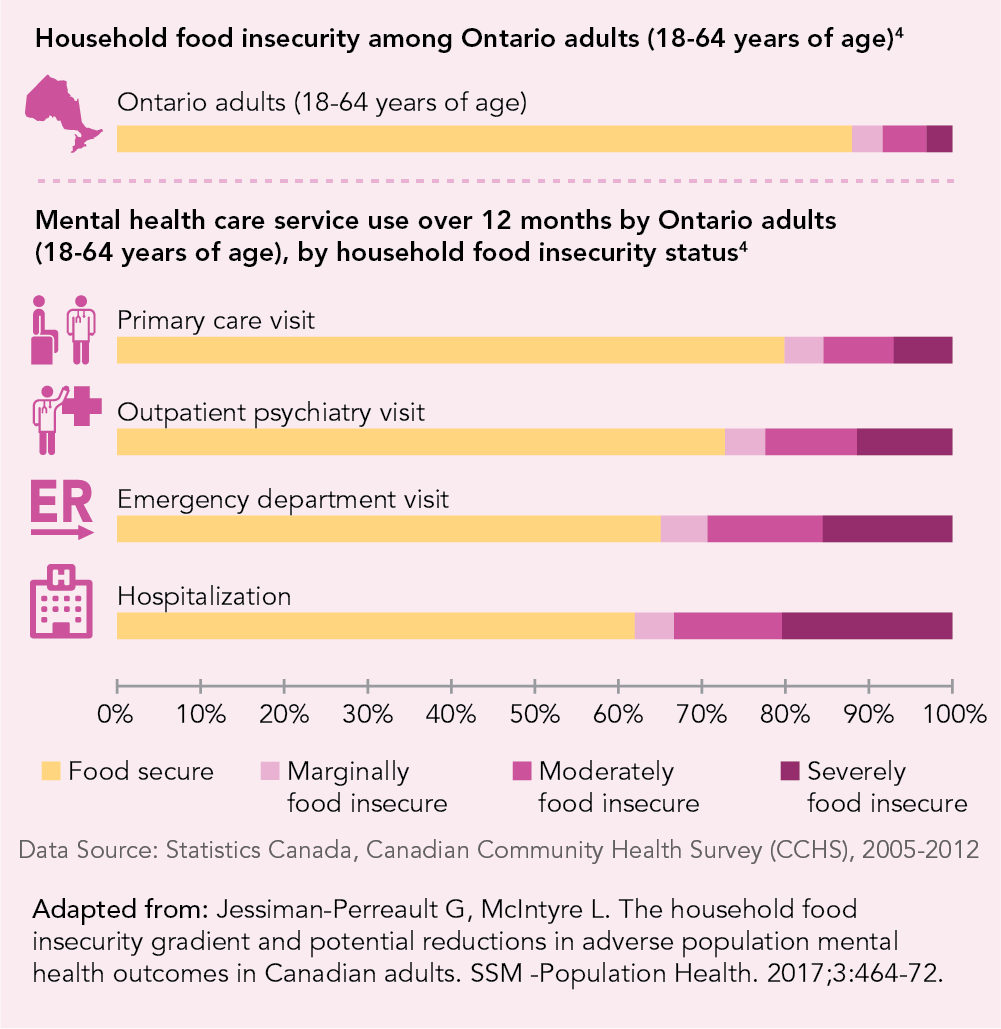
Evidence from Ontario shows that adults living in food insecure households put a large burden on mental health care services.4
While 1 in 8 households in Ontario is food insecure, adults living in food insecure households account for more than 1 in 3 hospitalizations due to mental health problems.
More severe food insecurity is associated with higher odds of mental health care service utilization and this relationship remains even after accounting for prior care for mental health reasons.
The co-existence of food insecurity and mental health problems is highly detrimental. Food insecurity makes it difficult for individuals to manage chronic mental health problems, while mental illness can impede their ability to become food secure.8
Food insecurity can be reduced through public policies that improve the financial circumstances of low-income households, such as increased social assistance benefits or guaranteed annual income like the public pensions afforded to seniors.9, 10
Research has shown that receiving a guaranteed annual income can alleviate mental health problems and the burden on our healthcare system.11, 12 An evaluation of Mincome, the guaranteed annual income project in Manitoba during the 1970s, found decreased mental health care utilization following its implementation.12
References
- Tarasuk V, Mitchell A, McLaren L, McIntyre L. Chronic physical and mental health conditions among adults may increase vulnerability to household food insecurity. J Nutr. 2013;143(11):1785-93. https://academic.oup.com/jn/article/143/11/1785/4571730
- Jessiman-Perreault G, McIntyre L. The household food insecurity gradient and potential reductions in adverse population mental health outcomes in Canadian adults. SSM -Population Health. 2017;3:464-72. https://www.sciencedirect.com/science/article/pii/S2352827316301410
- Tarasuk, V., Cheng, J., de Oliveira, C., Dachner, N., Gundersen, C., & Kurdyak, P. (2015). Association between household food insecurity and annual health care costs. Can Med Assoc J. 187(14), E429-E436. http://www.cmaj.ca/content/187/14/E429.full
- Tarasuk V, Cheng J, Gundersen C,de Oliveira C, Kurdyak P.The relation between food insecurity and mental health care service utilization in Ontario. Can J Psychiatry. 2018. https://journals.sagepub.com/doi/10.1177/0706743717752879
- Melchior M, Chastang J, Falissard B, Galera C, Tremblay R, Cote S, et al. Food insecurity and children’s mental health: a prospective birth cohort study. PLoS One. 2012;7(12):e52615. http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0052615
- McIntyre L, Williams J, Lavorato D, Patten S. Depression and suicide ideation in late adolescence and early adulthood are an outcome of child hunger. J Affect Disord. 2012;150(1):123-9. https://www.sciencedirect.com/science/article/pii/S0165032712007823
- McIntyre L, Wu X, Kwok C, Patten S. The pervasive effect of youth self-report of hunger on depression over 6 years of follow up. Soc Psychiatry Psychiatr Epidemiol. 2017;52:537-47. https://link.springer.com/article/10.1007%2Fs00127-017-1361-5
- Lent M, Petrovic L, Swanson J, Olson C. Maternal mental health and the persistence of food insecurity in poor rural families. J Health Care Poor Underserved. 2009;20(3):645–661. https://muse.jhu.edu/article/270008
- Loopstra, R., Dachner, N., & Tarasuk, V. (2015). An exploration of the unprecendented decline in the prevalence of household food insecurity in Newfoundland and Labrador, 2007-2012. Canadian Public Policy, 41(3), 191-206. https://www.utpjournals.press/doi/abs/10.3138/cpp.2014-080
- McIntyre L, Dutton D, Kwok C, Emery J. Reduction of food insecurity in low-income Canadian seniors as a likely impact of a Guaranteed Annual Income. Can Pub Pol. 2016;42(3). https://www.utpjournals.press/doi/abs/10.3138/cpp.2015-069
- McIntyre L, Kwok C, Emery JC, Dutton DJ. Impact of a guaranteed annual income program on Canadian seniors’ physical, mental and functional health. Can J Public Health. 2016;107(2):e176. http://journal.cpha.ca/index.php/cjph/article/view/5372
- Forget E. The town with no poverty: the health effects of a Canadian guaranteed annual income field experiment. Can Pub Po. 2011;37(3):283–305. https://utpjournals.press/doi/abs/10.3138/cpp.37.3.283