The household food insecurity gradient and potential reductions in adverse population mental health outcomes in Canadian adults
June 12, 2017
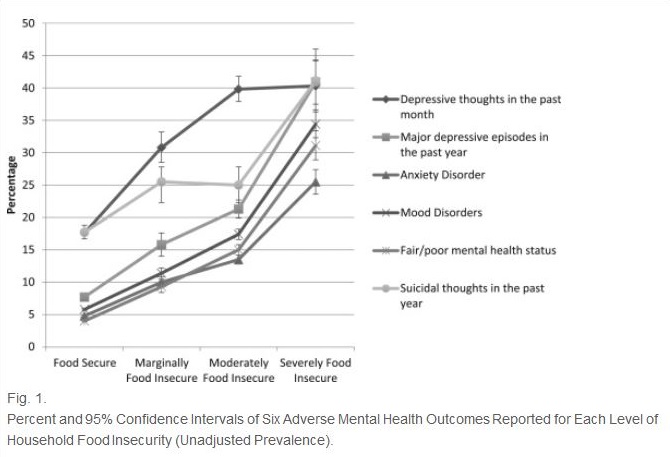
This study furthers our understanding of the relationship between household food insecurity and poor mental health by examining the relationship between the severity of household food insecurity and six mental health outcomes in a large pooled sample of adults (18-64 years old) drawn from the Canadian Community Health Survey (n=302,683). The mental health conditions under study included: major depressive episodes in the past year, depressive thoughts in the past month, anxiety disorders, mood disorders, self-reported mental health status and suicidal thoughts in the past year.
Findings showed a food insecurity gradient across each of the adverse mental health outcomes – the odds of reporting an outcome increased with the severity of food insecurity. The odds of reporting mental health conditions among adults in severely food insecure households were very high (25.5% to 41.1%, depending on the condition), and the researchers calculated that a decrease of between 8.1% and 16.0% in the reporting of these mental health outcomes would accrue if those who were severely food insecure became food secure. The results of this study suggest that macro-level policy interventions that reduce the severity of food insecurity, particularly severe food insecurity, could reduce mental ill-health burden.